• BEFORE THE OPERATION
An examination followed by an examination of the skin lesion or scar offending has been achieved by the surgeon to specify or possibility (s) Surgical (s).
In case of purely "local" anesthesia time, a pre-anesthetic assessment can be prescribed and preoperative consultation must be scheduled with the anesthetist.
No medication containing aspirin should not be taken within 10 days before surgery.
It is best not to smoke or drink alcohol the day before surgery.
Depending on the type of anesthesia, you may be asked to remain fasting (eat or drink) 6 hours before surgery.
No makeup and no jewelry or piercing should only be worn during the operation.
• TYPE OF ANESTHESIA AND CONDITIONS OF HOSPITAL
Type of anesthesia: Three methods are possible:
Local anesthesia pure analgesic where a product is injected to ensure the insensitivity of the area to be operated. This is the most common case for Dermatologic Surgery basis.
Anesthesia "vigil" (local anesthesia depth by tranquilizers), during which you can stay awake but relaxed and you will which may result in some amnesia intervention. It may be preferred for reasons of personal convenience or to achieve some complex ragged, especially on the face.
General anesthesia classic, in which you sleep completely, rarely useful Dermatological Surgery
The choice between these techniques is the result of a discussion between you, the surgeon and the anesthetist.
Type hospitalization interventions Dermato-surgery basis, especially if they are provided under local anesthesia, does not necessarily require hospitalization and can, like dental care, be made by Cabinet, insofar all necessary equipment is available.
If the intervention is scheduled for clinic or hospital, it can usually be used "externally", that is to say with an entrance just before the operation and exit just after it, or " outpatient ", that is to say" day hospital "with out the same day after a few hours of monitoring.
The traditional hospitalization, with one night to go there, is exceptional for this type of surgery.
• AFTER THE INTERVENTION: THE OPERATING SUITES
One can possibly see some discomfort with a feeling of tension on the scar but real disabling pain are rare. The first few days it will avoid "force" on the scar. Caution should be exercised vis-à-vis movements too would seek the operative area. In the following the procedure, a small seepage of blood (red) or lymph (yellow) hours may possibly come slightly stain the dressing. In the first 48 hours, the operated area can sometimes reveal edema (swelling) and small bruises (blue), which are only temporary. Itching are also quite common during the healing phase. All these findings are not
concern and should be considered "normal" suites. The son, when they are not absorbable, are removed between the 5th and 15th day.
The scar will then be massaged as directed by your surgeon.
Scar on the evolution usual, it should be noted that initially the scar is often red or pink, then it may turn brown and become fibrous, indurated, before clearing and soften after a few weeks to month, usually in fact beyond the third month after surgery.
On exposure to the sun, as the scar is still dark, it is best to avoid exposure and use a "full screen" type protection.
• THE RESULT
A period of several months (sometimes up to one to two years) is necessary to assess the final appearance of the scar.
It is important to understand that healing is a random phenomenon whose quality can never be guaranteed. The technical mastery of a skilled surgeon and specifically trained for this type of intervention allows plastic put the odds on his side but does not eliminate this randomness.
Under a surgical correction of abnormal scar, it is essential to regularly monitor the development and appearance of the scar. This is the only way to be sure to identify potential problems in time to healing and to apply appropriate treatment.
• DEFECTS AND POTENTIAL PROBLEMS
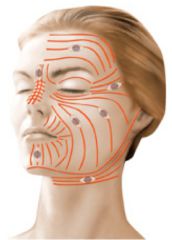
Although every effort will be implemented during and after the operation to make the most discrete scars possible, sometimes the healing is not at the height of efforts, and the resulting effects are more visible than what was expected. Indeed, the quality of healing is highly variable depending on the age, body parts, environmental factors, and a
patient to another. This is because, as we have seen, by the fact that the healing process involves quite random phenomena, sometimes unpredictable and incompletely controllable. In this regard, we must not forget that if the surgeon who performs the suture, the scar, it is the fact of (the) patient (s). The occurrence of an unsightly scar, however, must be submitted to your surgeon as it may lead to consider the use of certain therapeutic means.
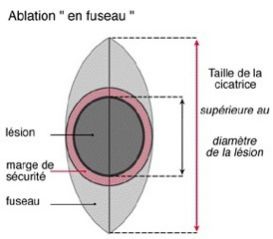
After removal of a malignant skin lesion, pathological microscopic examination can sometimes conclude that the margin of safety at its periphery was insufficient and that the lesion, whose boundaries are blurred and sometimes very difficult to determine precisely the eye naked, would therefore can not be removed completely or with a sufficient safety margin. Revision surgery to remove any remaining tumor or to spend more remote former lesion is the most essential time.
Although the removal of a lesion was considered complete, including pathological examination can sometimes help, even years later, a local "recurrence" of injury. This is explained by the fact that some lesions are "multifocal", ie they have several buds developing some of which may be small, undetectable during the first intervention, and
noncontiguous to main lesion. They can be initially saved and then develop their own behalf.
The Dermatologic Surgery is interventions "surface" which concern only the skin and are therefore not very "heavy". However, they have, like any medical procedure if it is minimal, a number of uncertainties and risks.
By choosing a qualified and competent plastic surgeon, trained specifically for this type of technology, you limit these risks, but did not completely remove.
Fortunately, significant complications are rare after intervention skin surgery performed within the rules. In practice, the vast
majority of happens without any problems and patients are fully satisfied with their operation. However, despite their rarity, you should be aware of possible complications:
• Anesthetic Complications: be aware that any anesthesia whatsoever (even local), induced in the body of the unpredictable and sometimes more or less easy to control reactions. It is unnecessary and impossible to mention all these complications but we urge you to discuss with the anesthetist (if it occurs) at its pre-operative consultation and ask him, on this occasion, all the information that you deem necessary . However, keep in mind that the techniques, anesthetics and monitoring methods have made tremendous progress over the past twenty years, and that the risks have become almost negligible, especially when the operation is carried out of urgency in a person free from any disease, let alone when it comes to local anesthesia where the very rare reactions are often limited to a simple little minor discomfort.
• Small bleeding: they can occur even a few days after surgery. They are usually easy to control.
• Hematoma: mostly harmless, they can prove to be evacuated if they are too large.
• Infection: it can be linked to a form of intolerance son suture or be favored by the presence of a small hematoma. It is characterized by intense pain and local redness with purulent discharge. The use of antibiotics or simple local health permit, most of the time, solve the problem, sometimes with negative consequences on the quality of the scar.
• Skin necrosis: it is a mortification of the default skin blood supply. It is exceptional and occurs only in cases of extreme tension on the banks of the scar or when making a flap to the precarious vascularization. It can sometimes complicate a hematoma or infection. It is much favored by smoking. It seriously compromises the aesthetic result.
• Failure of engraftment: a successful transplant is never 100% certain. It may therefore sometimes attend necrosis, mostly partial time of transplantation.
• Abnormal healing: beyond unsightly scars already mentioned, we think the most rare but deadly scars "keloid" true, the treatment is very difficult and often disappointing.
• Injury to nearby nerves: the more often it is the sensory nerve fibers that are involved, then leading to localized disturbances of sensibility (anesthesia, tingling ...).
Exceptionally at the front, it may be a motor branch, resulting in partial paralysis of the face concerned (eg half the forehead). Fortunately most of the time these problems are transient and disappear spontaneously within a few weeks.
In total there should not overstate the risks, but just be aware that surgery, even seemingly simple, still a small share of hazards. The use of a qualified Plastic Surgeon ensures that it has the training and knowledge required to avoid these complications, or effectively treat if jurisdiction.
These are the pieces of information that we wanted to bring you in addition to the consultation. We recommend that you keep this document, read it again after the consultation and reflect "a clear head." This reflection may raise new questions for which you wait for additional information. We are available to talk during the next consultation, or by phone, or even on the day of surgery when we meet in any way before anesthesia.
SKIN SURGERY



AESTHETIC PLASTIC
& RECONSTRUCTIVE SURGERY

© Docteur Garson MAJ 2013